Mini Gastric Sleeve Weight Loss Surgery: Benefits, Potential Risks
-
 Written by
Michael J. Ormsbee
Written by
Michael J. Ormsbee
- LAST UPDATED October 23, 2023
As global obesity rates have surged, a growing number of individuals are opting for bariatric surgery to assist with weight loss. Among the available procedures, the mini gastric sleeve has gained traction for its effectiveness in facilitating substantial weight loss, while also being a relatively low-risk and non-reversible restrictive option.
What is a Mini Gastric Sleeve?
The mini gastric sleeve is a modification of the traditional gastric sleeve surgery. It is considered a minimally invasive form of bariatric surgery that promotes weight loss by surgically reducing the size of the stomach.
In a traditional sleeve gastrectomy, around 75-80% of the stomach is removed, leaving a narrowed sleeve-shaped portion of the stomach intact. This smaller remaining stomach pouch restricts the amount of food that can be consumed by limiting the reservoir capacity. Removing the majority of the stomach also means less of the appetite-stimulating hormone ghrelin is produced, which aids weight loss.
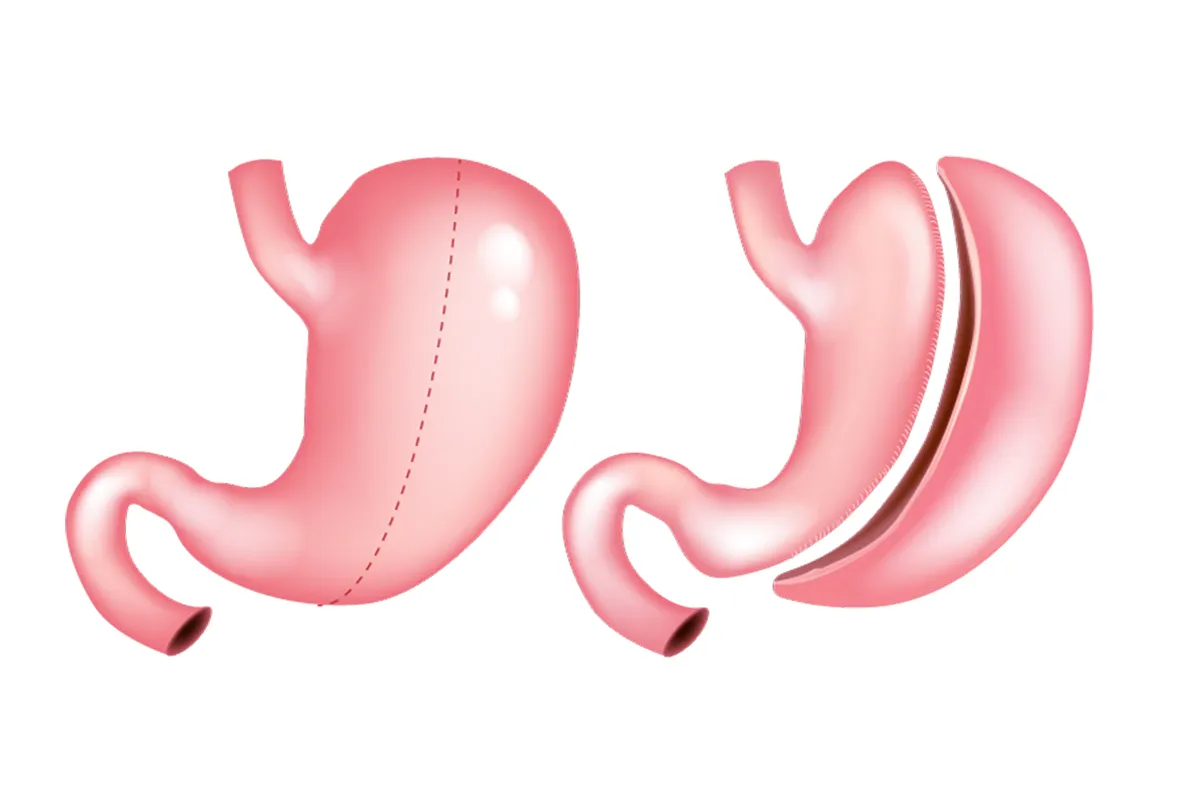
The mini gastric sleeve follows a similar principle but removes less of the stomach than the traditional procedure – around 50-70% rather than 75-80%. It is considered “mini” because it preserves more stomach tissue. However, the mini sleeve still substantially downsizes the functional volume of the stomach so that patients experience early satiety when eating and cannot consume large portions.
The reduced stomach capacity promotes quick weight loss by physically restricting food intake. At the same time, hormone changes that result from removing a section of the stomach may help reduce hunger and appetite. By making overeating difficult coupled with appetite suppression, significant weight reduction is typically achieved.
Ideal Candidates for Mini Gastric Sleeve Surgery
The mini gastric sleeve is best suited for individuals who:
- Have a body mass index of 30 or higher, making them clinically obese. Generally, candidates should be at least 30 pounds overweight.
- Have failed to achieve or maintain weight loss through traditional non-surgical methods such as dieting and exercise.
- Do not have serious health conditions that might be immediately life-threatening if not treated with rapid, dramatic weight loss.
- Do not have a history of extensive prior abdominal surgeries, which increase risk.
- Do not exhibit problematic eating disorders such as binge eating or night eating syndrome.
- Are motivated and ready to make the comprehensive diet and lifestyle changes required after surgery for long-term success.
Some considerations may make a patient unsuitable or less than ideal for the mini gastric sleeve. They include:
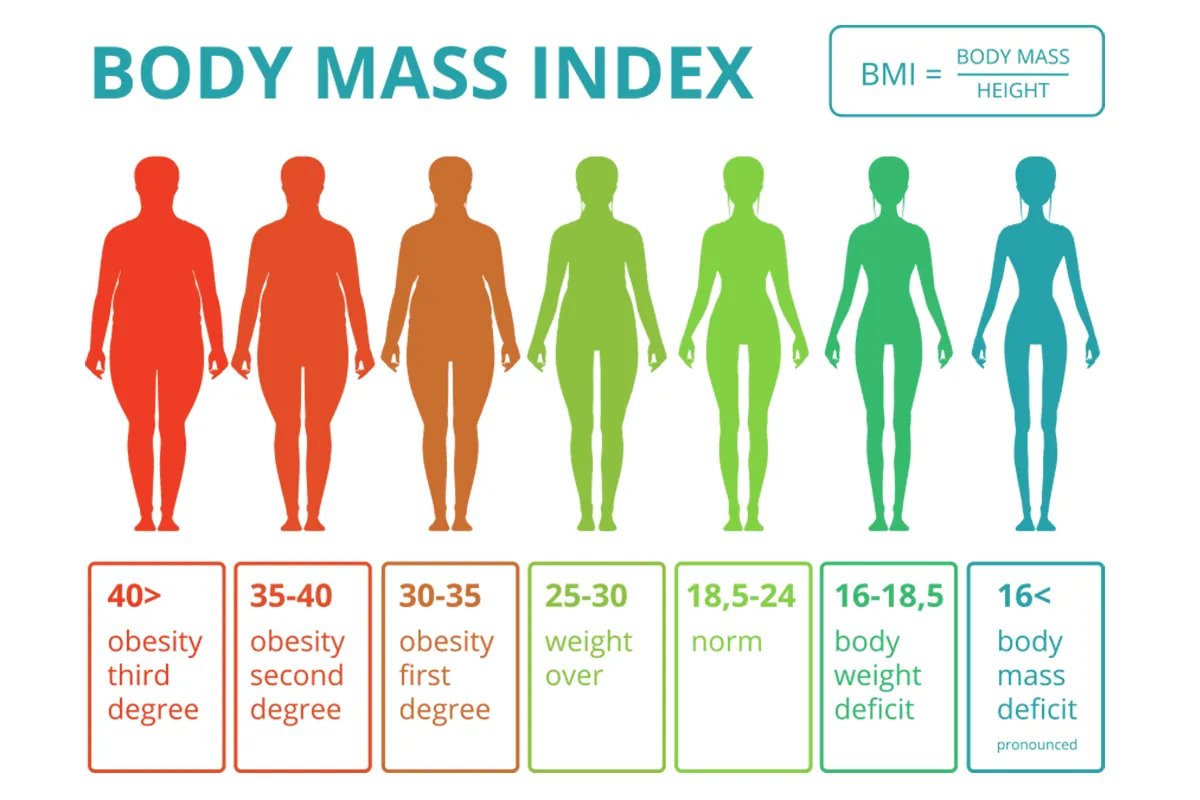
- Advanced obesity with a BMI over 50. For these super-obese patients, a more aggressive malabsorptive weight loss procedure may be recommended instead.
- Multiple complex medical conditions in addition to obesity. Candidates need to be healthy enough to undergo surgery.
- Current pregnancy or plans to get pregnant within 18 months of surgery. Weight loss from surgery can risk fetal development.
- Active substance abuse issues. This may interfere with the ability to make needed lifestyle adjustments.
- Unresolved binge eating disorder or emotional eating habits. These require targeted behavioral treatment pre-surgery.
- Inadequate social support system. Support is needed for following post-op diet and care guidelines.
The Mini Gastric Sleeve Procedure
The mini gastric sleeve procedure is a minimally invasive surgical technique characterized by the use of an endoscopic camera and specialized instruments, inserted through small incisions. This method stands in contrast to traditional open surgeries, which employ a single large incision. The small incisions associated with the mini sleeve surgery result in less pain, fewer complications, and a faster recovery.
The steps involved in the mini gastric sleeve surgery are as follows:
See Also:
- The surgeon begins the mini sleeve surgery procedure by making 5-6 small incisions in the abdomen in order to place ports for both camera and surgical instruments.
- The abdomen is inflated using carbon dioxide gas, providing a clearer vision and working space for the surgeon.
- The next step in the mini gastric sleeve is to segregate the blood vessels supplying the larger section of the stomach’s greater curvature.
- Removal of 50-70% of the stomach follows, achieved by cutting off its blood supply and then using surgical staplers to divide it.
- The excised stomach part is then extracted via one of the incisions, a unique aspect of the mini sleeve surgery.
- The surgeon then conducts a thorough inspection to ensure that there are no signs of bleeding and to verify the integrity of the newly formed slimmed-down stomach sleeve.
- The closing stages of the mini gastric sleeve procedure involve the irrigation of the abdominal cavity, removal of the instruments, and finally stitching or gluing of the incisions.
The entire procedure, or mini gastric sleeve surgery typically lasts just 60 to 90 minutes. The usual stay in the hospital after a mini sleeve surgery operation is 1-2 nights before the patient can be released for convalescence at home.
Benefits of the Mini Gastric Sleeve Procedure
Some of the advantages that make the mini sleeve an appealing weight loss surgery option include:
Less Invasive Surgery
The minimally invasive laparoscopic technique used for the mini gastric sleeve requires only tiny incisions rather than cutting completely open the abdomen. This results in significantly reduced pain, lower risk of infection, less scarring, and faster recovery compared to open surgery. Most people can return to normal daily activities within 2-3 weeks versus 2-3 months with traditional invasive surgery.
Lower Risk Profile
The mini sleeve has a lower risk of both surgical complications and long-term nutritional deficiencies compared to malabsorptive procedures like gastric bypass or duodenal switch surgery. Because it solely limits food intake without interfering with digestion and nutrient absorption, risks are reduced. For example, there is no risk of “dumping syndrome” which can happen after gastric bypass.

Rapid Weight Loss
Most patients lose 50-70% of their excess body weight within 6-9 months after the mini gastric sleeve procedure. For example, a 300-pound person may expect to lose 100 pounds or more. The restrictive capacity of the smaller stomach pouch promotes weight loss quickly once solid foods are reintroduced after a liquid diet healing period.
No Malabsorption Issues
By simply reducing stomach volume rather than rerouting the intestines, the mini gastric sleeve does not affect the normal absorption of calories and nutrients from food. This avoids potential complications like protein deficiency, iron deficiency, and vitamin deficiency that can occur with malabsorptive procedures. Patients can generally continue eating a well-balanced normal diet without needing supplemental vitamins long term.
Reversibility
The mini sleeve surgery does not permanently alter digestion like gastric bypass or duodenal switch and therefore can be reversed if needed. Conversion to another bariatric surgery is possible. However, reversing the mini sleeve involves an additional major surgery and is rarely indicated unless complications develop.
Mini Gastric Sleeve of Potential Drawbacks and Risks
Possible disadvantages and negative outcomes that need to be considered before choosing the mini sleeve include:
Acid Reflux
A significant portion of patients develop chronic acid reflux after the mini gastric sleeve, which can require long-term medication. This happens because removing part of the stomach reduces its acid-producing cells. The small sleeve pouch also empties directly into the intestine, making reflux more likely.
Weight Regain
While significant weight loss is achievable in the 1-2 years after surgery, weight can creep back up without major diet and lifestyle adaptations. If eating habits revert to high-calorie, high-fat, high-sugar foods, weight regain is likely without the ability to consume large volumes.
Surgical Complications
As with any surgery, risks during or soon after the procedure include bleeding, infection, blood clots, leaks from the staple line, or adverse reactions to anesthesia. These occur in less than 5% of mini gastric sleeve surgeries but can result in serious consequences if they do occur. Strictly following post-op guidelines can help minimize risks.
Hospital Readmission
Around 7% of mini sleeve patients require readmission to the hospital in the 30 days following discharge, commonly for dehydration, nausea, vomiting, or high fever indicating an infection or other surgical complication. Following directions for nutrition, hydration, incision care, and limiting activity is essential to avoid issues.
Mini Gastric Sleeve Comparison to Other Bariatric Surgery Procedures
The Mini Gastric Sleeve is a popular bariatric surgery procedure known for its restrictive approach toward weight loss. To better understand its benefits and drawbacks, let’s compare it with some other common weight loss surgeries.
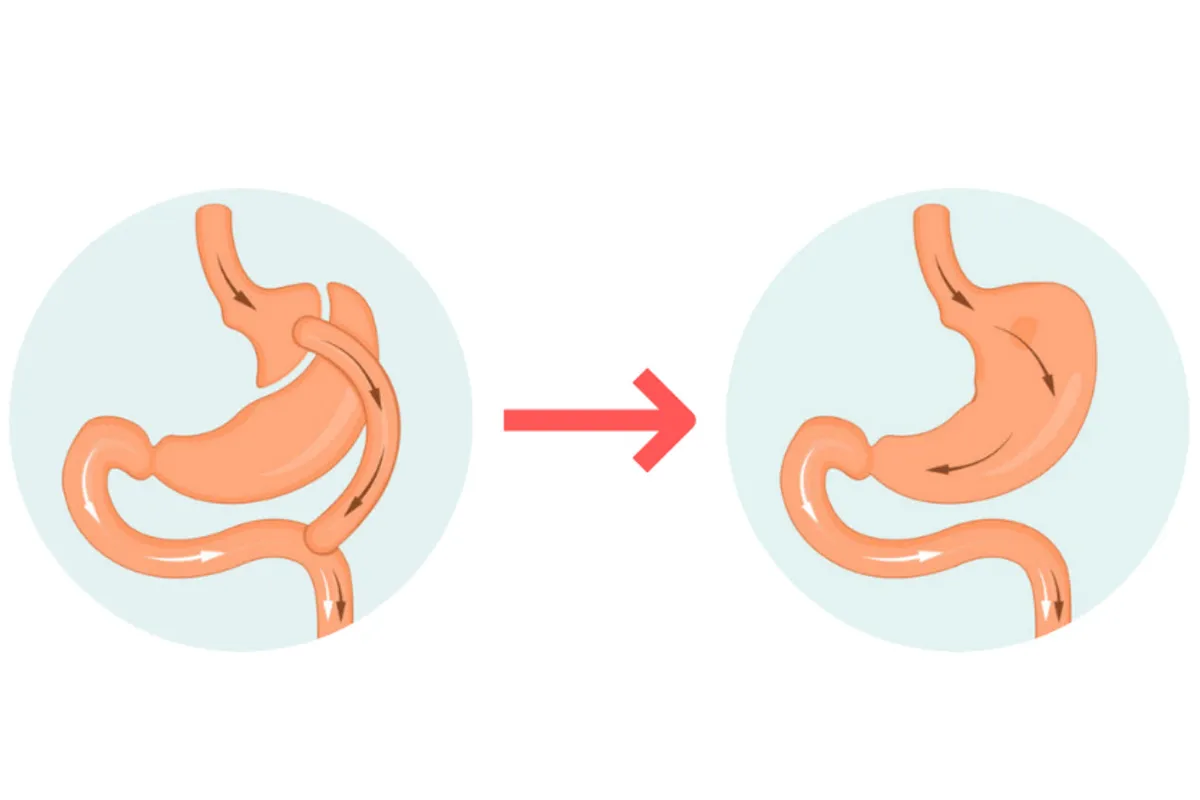
Gastric Bypass
In comparison, Gastric Bypass is both a restrictive and malabsorptive procedure. While it reduces the stomach’s capacity like the mini gastric sleeve, it also reroutes part of the small intestine. This additional step typically results in more significant weight loss compared to the mini sleeve. However, the variation in nutrient absorption can lead to higher risks of nutrient deficiencies. Moreover, the surgery presents a greater possibility for “dumping syndrome,” a condition that causes food to move from the stomach to the small bowel too quickly.
Lap Band
Lap Band surgery or Adjustable Gastric Banding contrasts the mini sleeve by focusing solely on restriction. Instead of removing a part of the stomach, an inflatable band is placed around it. The flexibility of the band allows adjustments according to the patient’s needs and can even be reversed. However, the weight loss with a lap band is typically slower and often less successful in the long term compared to the mini sleeve.
Biliopancreatic Diversion
The Biliopancreatic Diversion with duodenal switch is a malabsorptive procedure that greatly reduces nutrient absorption, posing a significant risk for long-term vitamin and mineral deficiencies. The amount of weight loss experienced is substantial, similar to the gastric bypass but more so than the mini gastric sleeve. Nevertheless, due to its high risk, it may not be a suitable choice for all patients.
Vertical Gastric Sleeve
The Vertical Gastric Sleeve, although similar in name, differs in its approach to the mini gastric sleeve. This procedure drastically reduces stomach size, eliminating the portion responsible for producing the hunger hormone, Ghrelin. Even with its promising weight-loss prospects, it doesn’t assure the same level of stomach capacity preservation the mini sleeve provides.
Gastric Balloon
A less invasive procedure compared to the aforementioned ones is the Gastric Balloon. A silicone balloon is inserted endoscopically and then inflated to decrease the available stomach space. Although this option is entirely reversible and requires no incisions, its weight loss potential is considered the least among these procedures – less adequate for severe obesity cases.
The mini gastric sleeve offers balanced, significant weight loss outcomes with fewer risks and complications when compared to other procedures. Despite these advantages, it is important to note that its success depends largely on patients’ commitment to essential lifestyle and dietary changes following the surgery. Each of these procedures has its unique benefits and challenges – targeting various patient needs and health considerations.
The mini gastric sleeve, due to its less invasive nature and reasonable weight-loss quality, often presents itself as a suitable option for many opting for bariatric surgery. However individual health factors, obesity levels, and weight loss goals should always be evaluated by healthcare professionals to determine the most beneficial route.
Mini Gastric Sleeve Before and After
The mini gastric sleeve procedure typically enables patients to lose 50-70% of their excess body weight over the first 1-2 years after surgery. The average person will lose around 60% of excess weight as early as 12-18 months post-op.
For example, if a patient’s ideal body weight is calculated to be 150 pounds, and they weigh 250 pounds pre-surgery, they have 100 pounds of excess weight. This person could expect to lose about 60-70 pounds in the first 1-2 years after a mini sleeve, achieving a weight closer to 180 pounds eventually.
Rapid weight loss begins in the 2-3 months after surgery as the body adjusts to the smaller stomach capacity. Monthly weight loss generally averages around 5-8 pounds during this rapid phase. As the maximum loss is achieved, monthly weight loss then levels off to 1-3 pounds on average to sustain an optimal weight.
Beyond the numbers on a scale, most mini gastric sleeve patients experience drastic improvements in underlying conditions like high blood pressure, diabetes, sleep apnea, joint pain, and cholesterol with successful weight reduction. Many are able to discontinue or reduce medications for these conditions. Mobility and stamina also increase remarkably for most individuals as their health improves post-surgery.
Gastric Sleeve vs. Gastric Bypass
The mini gastric sleeve and gastric bypass are two of the most commonly performed bariatric surgery procedures. They contrast in several key ways:
| Comparison Aspect | Mini Gastric Sleeve | Gastric Bypass |
|---|---|---|
| Weight Loss Amount | 60% - 70% excess weight loss | 70% - 80% excess weight loss, patients often lose weight more quickly and reach a lower final weight |
| Surgical Risk | Lower overall surgical risks | More complex surgery with higher risk of complications, such as intestinal leaks |
| Side Effects | No malabsorption issues | Risk of vitamin deficiencies and "Dumping Syndrome" due to malabsorption |
| Reversibility | Reversible when required | Permanent changes to the digestion route |
| Best Fit For | Depends on an individual's health profile, needs, and goals. This procedure might be preferred by younger patients who want to avoid permanent changes | Although higher risks, the more significant weight loss may be necessary for high-risk patients |
Please remember that the best course of action should always be decided in consultation with an experienced bariatric surgical team, who can consider individual health profiles, patient’s specific needs, and goals.
Mini Gastric Sleeve 10 Years Later
The mini gastric sleeve procedure provides effective weight loss for the majority of patients in the short term 1-3 years after surgery. However, maintaining long-term weight loss requires significant diet and lifestyle adaptations. Without these sustained behavior changes, weight regain is very common 7-10 years later.
One study in the journal Obesity Surgery followed mini gastric sleeve patients for 10 years after their procedures. Results showed:
- After 10 years, the average weight regain was about 50% of the maximal weight lost.
- However, the average weight after 10 years was still 28% lower than the original pre-surgery weight.
- About 20% of patients maintained successful weight loss after 10 years.
- Most weight regain occurred between post-op years 3 through 6.
This indicates the mini sleeve can facilitate weight control in the long term, but patients must remain vigilant with lifestyle changes to avoid recidivism. Strictly following the recommended post-op diet, exercising consistently, limiting alcohol intake and sweets consumption, and ongoing nutrition counseling maximize lasting success.
Some mini gastric sleeve patients do opt to undergo a second revision surgery such as gastric banding or conversion to gastric bypass if they begin to regain their weight after 5 or more years. However, revision surgery options should not be viewed as a quick fix for resuming poor eating and exercise habits. Comprehensive lifestyle and behavior modifications remain essential for long-term weight maintenance after bariatric surgery procedures.

Making the Decision: Is Mini Gastric Sleeve Right for You?
The mini gastric sleeve is one effective surgical option for enabling significant weight loss, but success requires full commitment to post-op lifestyle changes. Thoroughly researching the procedure, its benefits relative to risks, and what will be expected after surgery is imperative.
Important factors to consider include:
- Your weight loss goals and the amount of excess weight to lose.
- Your current medical conditions and any special nutritional needs.
- Your willingness and ability to adhere to major diet, exercise, and behavior changes.
- Your personal tolerance for surgical risk and potential complications.
- Your expectations for life after surgery and motivation to make this lifelong commitment.
Finding an experienced bariatric surgery team you trust, and having honest, in-depth discussions of your situation, needs, and concerns, allows determine if the mini gastric sleeve is the most appropriate option for you. This major decision requires delving deep into your individual circumstances and priorities. The surgery is simply a tool—the hard work of transforming your lifestyle is what sustains long-term weight loss and health.
Conclusion
With obesity levels rising, procedures like the mini gastric sleeve that promotes weight loss through restrictive stomach reduction are likely to continue growing in popularity. The mini sleeve offers potentially significant weight reduction for appropriate candidates who are ready to comprehensively overhaul ingrained lifestyle habits. While not entirely without risks, this minimally invasive approach avoids some of the nutritional and surgical complications of more complex bariatric surgeries. Patients who understand what to realistically expect from the mini sleeve surgery, and are prepared to put in the hard work making diet and fitness changes after surgery, can experience gratifying transformations in their health, mobility, and quality of life.

FAQs about Mini Gastric Sleeve
How much does a mini gastric sleeve cost?
The average cost of mini gastric sleeve surgery ranges from $8,000 to $15,000 depending on factors like the surgical facility, doctor fees, and geographic location. Many patients also face additional costs for nutritional counseling, physical therapy, required medical tests before surgery, and post-op follow-up care. Those with inadequate insurance coverage can expect to pay $10,000 to $20,000 or more out-of-pocket for the full costs associated with the procedure and recovery process. Financing options like medical loans are available, but patients should budget carefully and get cost estimates upfront before undergoing a mini sleeve.
Can I get a mini gastric sleeve?
You may be a candidate for the mini gastric sleeve if your body mass index is 30 or higher (or 27-29 with obesity-related health issues), you have struggled to lose weight through diet and exercise alone, you do not have complicating health factors, you are prepared to make major lifestyle changes, and you understand the risks and benefits of surgery. Important steps are consulting with a bariatric surgeon about your medical history and goals, having any needed conditions evaluated and stabilized, completing pre-op diet and lab requirements, ensuring you have practical and social support, and committing fully to post-op guidelines for nutrition, exercise, and follow-ups. The mini sleeve may not be advisable depending on your overall health status and BMI. Discuss your situation thoroughly with your bariatric team.
Is a mini gastric sleeve worth it?
For appropriate candidates, the mini sleeve can be an effective and lower-risk weight loss surgery option. When performed correctly by an expert bariatric surgeon, most patients lose 50-70% of excess body weight. However, success requires diligently sticking to the recommended post-op diet and implementing major nutrition, fitness, and lifestyle changes. If you are unable to make these lifelong commitments, the surgery may not be worth it. Risks include complications from surgery, acid reflux, weight regain, and the need for revision surgery later on. Get a full understanding of the benefits relative to short and long-term risks. Being ready to drastically adapt lifelong eating habits is key to determining if the mini sleeve is worthwhile.
How much weight can you lose with a mini sleeve?
Typical patients lose about 50-70% of their excess body weight within 12-18 months after the mini sleeve surgery. For example, if your excess weight is calculated to be 100 pounds, you could expect to lose 60-70 pounds. Most mini gastric sleeve patients continue to lose weight more gradually for up to 2 years after surgery, then maintain their lowest weight loss if they adhere to diet and exercise recommendations. Total weight loss depends on many factors including your starting weight, body composition, lifestyle habits, and any complications. Work closely with your bariatric team to develop realistic weight loss goals based on your unique profile if considering the mini sleeve.






